What Causes Melanoma?
Melanoma starts when mutations occur in the DNA of melanocytes, causing them to grow out of control. Several things can raise your risk:
- UV exposure: This is the biggest factor, especially from too much sun or using tanning beds.
- Fair skin: People with lighter skin, blue or green eyes, and blonde or red hair have less melanin and are more vulnerable.
- Sunburns: Severe or blistering sunburns, especially during childhood or adolescence, can increase risk.
- Family history: If close relatives have had melanoma, your risk goes up.
- Past skin cancer: If you’ve had melanoma or another skin cancer before, recurrence is more likely.
- Lots of moles or unusual moles: Particularly large or irregular ones, called dysplastic nevi, are a concern.
- Weakened immune system: Whether from a health condition or medication (like after an organ transplant), a weaker immune system raises the risk.
- Genetics: Inherited gene mutations—especially in genes like CDKN2A or BRAF—can play a role.
While melanoma is more common in people over 50, it can affect younger individuals too. Men are slightly more likely than women to get it, and it’s especially widespread in places with strong UV rays—think Australia and New Zealand.

How Is Melanoma Diagnosed?
If a mole or skin spot looks concerning, a dermatologist will usually do a few things:
- Visual check: They’ll use a special device called a dermatoscope to closely inspect the spot.
- Skin biopsy: This is the only way to confirm melanoma. A sample of the skin is taken and looked at under a microscope.
- Histopathology: This analysis looks at key features of the tumor, such as:
– Breslow thickness (how deep the tumor is),
– Whether there’s ulceration,
– The mitotic rate, or how fast cells are dividing.
If advanced melanoma is suspected, imaging tests might be needed:
- Ultrasound or CT scans: To see if nearby lymph nodes or organs are affected.
- PET or MRI scans: These help detect spread to distant organs.
- Sentinel lymph node biopsy: A surgical test to see if cancer has reached nearby lymph nodes.
Stages of Melanoma
Melanoma is staged from Stage 0 (very early) to Stage IV (advanced), depending on how far it has spread.
- Stage 0 (in situ): The cancer is only in the top skin layer. Very treatable with surgery.
- Stage I–II: The tumor is thicker and possibly ulcerated, but hasn’t spread. Risk rises with size and depth.
- Stage III: The cancer has reached nearby lymph nodes or skin.
- Stage IV: It has spread to distant organs—like the lungs, liver, brain, or other parts of the skin.
Doctors use a system called AJCC TNM to describe melanoma:
- T = Tumor (size and depth)
- N = Node (lymph node involvement)
- M = Metastasis (spread to distant parts of the body)
Melanoma Prognosis
Your outlook depends a lot on how early the melanoma is found:
- Stage 0 & I: Great outcomes—over 90–99% 5-year survival rate.
- Stage II: Still treatable, but survival drops to around 70–85%.
- Stage III: Moderate prognosis, with survival rates between 40–78%, depending on how many lymph nodes are affected.
- Stage IV: More serious, but thanks to newer treatments like immunotherapy and targeted drugs, some people are now living much longer and even achieving remission.
 Advertisement:
Advertisement:continued on next page
Warum tragen manche Menschen ihren Ring am Mittelfinger?
Shrimp & Teriyaki Steak Noodles
Lamorne Morris Just Attended His First Emmys And Won All In The Same Night — I’m Not Crying, You Are
Just discovered this in my son’s hair. What is it? Not sure if we should go to doc
Raspberry Lemon Heaven Cupcakes
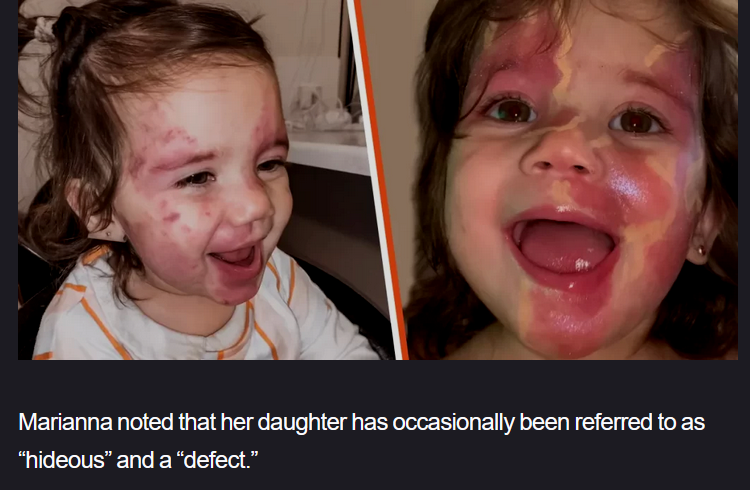
Baby Called “Hideous” and “Defective”